Thyroid Disorders & COVID-19

II ODISHABARTA II
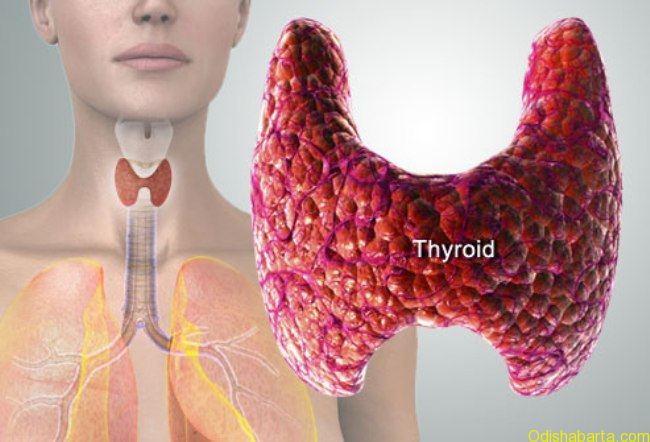
Thyroid disorders are second most common endocrine ailments next only to Diabetes. They occur in 10-12% of people. These are seen 5 times more commonly in females. Most common form is hypothyroidism (less hormone levels in blood) followed by hyperthyroidism (excess hormone levels in blood). As of now, there is not enough information regarding the relationship between thyroid disorders and susceptibility to COVID-19. Therefore currently there is no reason to believe that people with thyroid disease are at increased risk to contract this novel coronavirus, develop serious manifestations of infection or to experience complications.
Nevertheless, if thyroid medications are not taken as per prescription, uncontrolled thyroid disease may increase a person’s risk for viral infection and complications. Additionally, immunosuppressive drugs, high-dose steroids and certain other treatments can increase a person’s risk for infections and complications. People receiving these types of treatments should speak to their healthcare provider to ask about their specific risk.
In addition to following the general precautionary advices issued by different health authorities, individuals should observe specific guidance outlined below according to their thyroid condition.
Are individuals with autoimmune thyroid disease (hypothyroidism and hyperthyroidism) at increased risk of COVID-19 infection(?)
COVID-19 is a novel virus, so there is no information on how it affects individuals with thyroid disease. However thyroid disease is not known to be associated with increased risk of viral infections in general, nor is there an association between thyroid disease and severity, complications of viral infection.
Having autoimmune thyroid disease does not mean that a person is immune compromised or will be unable to fight off a viral infection. The part of the immune system that’s responsible for autoimmune thyroid conditions is separate to the immune system that’s responsible for fighting off viral infections, such as COVID-19. Patients who are classified as having a weakened immune system (immune compromised) are typically those with conditions such as leukemias, HIV and AIDS, or who are on medicines such as high-dose steroids, immunomodulatory drugs for rheumatoid arthritis or multiple sclerosis, cancer chemotherapy or following organ transplantation.
Does control of thyroid disease affect infection risk(?)
There is no evidence that those with poorly controlled thyroid disease are more likely to contract viral infections in general. However, it is possible that patients with uncontrolled thyroid disease (especially thyrotoxicosis) may be at higher risk of complications (like thyroid storm) from any infection. Patients with thyroid disease continue taking their thyroid medications to reduce this risk.
Does being on medication for thyroid disorder suppress immune system(?).
Neither levothyroxine, nor carbimazole nor propylthiouracil, are immunomodulatory therapies. i.e. they do not change nor weaken your immune system. However, some people with thyroid eye disease will be on high doses of steroid medication which can suppress the immune system.
What happens to a patient with Hyperthyroidism(?)
Although rare, anti-thyroid drugs (ATD) used to treat hyperthyroidism/ Graves’ disease may cause side effects that resemble symptoms of COVID-19, such as fever, sore throat, mouth ulceration and muscle pain, flu like illness as a result of a condition called agranulocytosis/ neutropenia (Decrease in white blood cell count). Here number of the immune cells that fight infection decrease. If you experience these symptoms, contact your endocrinologist or other healthcare provider (HCP) immediately and mention that you take thyroid medications. If these occur, patients are often told to stop the methimazole and go to a laboratory to have blood testing done. This is a complete blood count (CBC) to measure white cell count/differential.
Agranulocytosis is less common in patients who have been taking methimazole for a long time or when the dose of the medication is low (e.g. 15 mg in one study), but it can still occur. Research shows that the chance of a person taking carbimazole developing agranulocytosis is between 0.2- 0.5%.
It is recommended that all patients starting ATDs be given written information with instructions on what to do if they develop symptoms suggestive of neutropenia.
A patient infected with COVID-19 can continue ATDs unless neutropenia (absolute neutrophil count of < 1500 per microliter) is present. Of note, lymphopenia (reduction of lymphocyte count) seems common with COVID-19 infection and is not an indication to stop ATDs.
In resource limited setting, it may not be possible to check a CBC at the onset of symptoms suggestive of neutropenia. In this scenario, patients should stop the ATD and restart one week later if symptoms have resolved. If symptoms worsen during the period off ATDs or recur after recommencing the drug, the patient should seek urgent medical attention; in such situations performing a CBC is essential.
What should be the treatment of Thyroid Eye Disease (TED) in these times(?)
The general measures include avoidance of both active and passive smoking, usage of dark glasses under bright sunlight and artificial tear drops to prevent dry eyes.
Thyroid eye disease (TED) may be treated with high-dose steroids (immune suppressive dose) or other immune suppressants like mycophenolate (MMF), Rituximab. These people are extremely vulnerable and are at very high risk of viral infection, severity and complications. The patients should take steroid medication as prescribed and contact their endocrinologist or HCP to discuss the dosage during the COVID-19 pandemic. In some cases it may be prudent to temporarily suspend high-dose steroid or MMF treatment until the pandemic is over in consultation with your endocrinologist. This will depend on the severity of eye problem. The British Thyroid association advises these group of people to self-isolate/shield for at least 12 weeks.
Some individuals receive infusions as treatment for TED. Although rare, side effects from the infusion can resemble symptoms of COVID-19, including feeling hot, tachycardia, dyspnea and muscle pain. In case of occurrence of these symptoms, the healthcare provider should be contacted immediately and be informed about the treatment.
Individuals receiving steroids or infusions for TED may also experience hyperglycemia and should follow COVID-19 precautions outlined for people with diabetes.
How can methimazole (ATD) be given to patients with critical illness(?)
Methimazole is an oral medication and stopping these medications can lead to worsening of hyperthyroidism. During a critical respiratory illness, especially when a ventilator (breathing machine) is required, a patient may not be able to take medications by mouth. When treatment of hyperthyroidism is necessary, different routes for giving methimazole may be used. The placement of a naso-gastric tube allows the same methimazole pill to be delivered to the gut (digestive system) in a patient who is unable to swallow. If the enteric route (through the stomach) is not available, these medications can be prepared for intravenous (IV) use. Enema or suppository formulations have also been used and require specific preparation.
How can hyperthyroidism be treated in the event of unavailability of thyroid blood testing facility(?).
In the event of difficulty in performing thyroid function tests during these times, hyperthyroidism patients may be shifted to a ‘block and replace’ course of treatment. This is where antithyroid drugs are given to block the thyroid from producing any thyroid hormone and then levothyroxine is given to replace the thyroxine the body should be producing. This is a way of maintaining very stable thyroid function in most people, provided you take the tablets as requested.
Is it safe to defer definitive (radioactive iodine or thyroid surgery) treatment for hyperthyroidism(?)
The non medical modes of treatment like Radio iodine therapy and Thyroid surgery should be deferred for the current period. These measures are acceptable and absolutely safe.
There is no evidence that patients who have recently had radioiodine or thyroid surgery for benign thyroid disease are at increased risk of COVID-19 infection. If you have recently undergone radioiodine treatment for hyperthyroidism, you may need to start levothyroxine treatment if you start to develop symptoms of hypothyroidism. In these circumstances you should seek advice from your doctor about when and how to monitor your thyroid function. If you have started levothyroxine treatment you will need to have followed up blood tests to ensure you are on the correct dose.
What happens to patients with Hypothyroidism(?)
Rarely the corona virus can multiply and destroy the follicular cells in the thyroid gland responsible for thyroid hormone production giving rise to worsening of symptoms. As such, in case of worsening of symptoms, it is necessary to check thyroid hormone levels.
Patients with hypothyroidism and other comorbidities such as diabetes, cardiac disease, and hypertension are at high risk for severe COVID-19 infection and such patients need to take more precautions.
At this time, there are no identified shortages of any types of these thyroid hormone replacement medications. However, in order to maintain social distancing and limit exposure to COVID-19, patients should consider obtaining a 90-day supply of prescriptions.
Is more frequent testing of thyroid function during these times in patients with Hypothyroidism(?)
The usual 3-6 monthly testing is only required. If any symptoms like excessive tiredness, lethargy, body aches, swelling of face & legs, constipation, menstrual disturbances etc, occur it can be tested after consulting with your doctor.
Any recommendations for thyroid function test in patients with COVID-19 infection(?)
In COVID-19 patients with existing thyroid disease and on thyroid medications, if there is no indication, thyroid function test (TFT) should not be repeated.
In COVID-19 patients admitted in the intensive care unit, routine TFT is not recommended. There is no benefit of levothyroxine treatment in patients with euthyroid sick syndrome.
Subacute Thyroiditis and COVID-19(?)
The corona virus can induce an inflammation in the thyroid gland giving rise to Thyroiditis. There may be fever, throat discomfort with tender thyroid. Here initially thyroid hormone level goes up followed by normalization of hormone levels. Sometimes thyroid hormone levels may fall below normal requiring hormone replacement,
Is it safe to delay a biopsy of thyroid nodule(?)
Most thyroid nodules are benign (not cancerous), but some nodules of a certain size that also have suspicious features on ultrasound may be advised to undergo a biopsy. Even if the thyroid nodule is found to be cancerous, there is usually little risk in delaying surgery to have it removed. Thus, it would also be generally safe to delay biopsy of the nodule unless your clinician strongly advises that it be done urgently.
Patients with Thyroid Cancer.
Are patients with Thyroid Cancer more prone for COVID-19 infection(?)
Ans- People who are undergoing cancer treatment meet the definition of being immunocompromised. However, unlike many other types of cancer, the majority of thyroid cancer patients are not receiving chemotherapy or other treatment that would deplete the immune system and cause them to be immunocompromised. Having a previous diagnosis of thyroid cancer and receiving thyroid hormone medication is not a known risk factor for getting COVID-19 or being more severely affected by it. However, individuals with metastatic thyroid cancer (papillary or medullary) may be at increased risk of viral infection or complications if they have lung metastases or if they are undergoing certain types of cancer treatment.
The rare thyroid cancer patients who are receiving chemotherapy medications or multikinase inhibitors (such as Lenvatinib or Sorafenib) as a part of thyroid cancer treatment, they would be considered at higher risk for severe illness due to COVID-19. Patients who have previously received external beam radiotherapy to the neck may be at increased risk of severe illness with coronavirus and should also consider self-isolating.
What happens to surgical management of Thyroid Cancer(?)
Ans- The most common initial treatment for thyroid cancer is surgery to remove the thyroid tumor. While surgery is necessary, most thyroid cancers are very slow-growing tumors, and the chance of thyroid cancer worsening if surgery is delayed by several months is extremely low. This is true even if there is spread of the thyroid cancer to local lymph nodes in the neck. For patients with cancers categorised as ‘low risk’ (where progression is considered to be slow) surgery may be delayed until a time when it is considered safer to proceed. Surgery may also be deferred for patients considered susceptible to severe COVID-19 disease if they acquire the infection or if they may need intensive care monitoring after surgery.
However, thyroid surgery would be essential and should be performed more urgently for patients with symptoms due to the size of the thyroid tumor, such as difficulty breathing or swallowing, or rapidly progressive cancers that are invading other parts of the neck, or if the biopsy showed aggressive forms of thyroid cancer, including anaplastic thyroid cancer and medullary thyroid cancer.
Radioactive Iodine therapy for patients with Thyroid Cancer(?)
Ans- Radioactive iodine (RAI) therapy is often used for thyroid cancer patients after having surgery and typically involves several visits to a doctor or healthcare facilities. RAI is often used to eliminate any remaining normal (non-cancerous) thyroid tissue or to decrease the chance of recurrence even when all thyroid cancer appears to have been surgically removed. Whilst the treatment itself does not increase the risk of infection, subsequent radiation protection issues would seriously complicate the care of any patient who subsequently became unwell with COVID-19. In most cases radioiodine therapy is not urgent and can be safely delayed. Delays of six months or even longer do not appear to negatively affect the course of thyroid cancer in patients. Therefore, the short delays expected from waiting until the current COVID-19 pandemic is over are unlikely to lower the effectiveness of the RAI treatment.
In general, treatment with RAI is more urgent for patients who have papillary or follicular thyroid cancer, who have distant metastases to the lungs or other body parts, particularly if growth of the metastases have been observed. Your health care provider will advise you when it is better to delay RAI treatment or when it is better to proceed with treatment despite the current pandemic.
Does Surgery or RAI therapy for patients with Thyroid cancer increase the risk of COVID-19 infection(?).
Ans- Patients who have previously received treatment for thyroid cancer such as surgery, with or without radioiodine (remnant ablation or radioiodine therapy), are not considered at higher risk of general viral (and therefore COVID-19) infection.
Can patients receive TSH suppressive therapy (?)
Ans- Patients on suppressive doses of thyroxine (i.e have a TSH target of <0.1mU/l) should continue on their current dose. Being on suppressive dose of levothyroxine does not increase the risk of COVID-19 infection.
Dr Sunil Kumar Kota,MD (Med), DNB (Endo)
Consultant Endocrinologist, DIABETES & ENDOCARE Clinic, Berhampur Email: [email protected], Ph: +917749804401











